Life through a TV Screen PT. 3
***Disclaimer: This next chapter will be part personal experience, part physical therapy education based on existing research literature. It is not necessarily medical advice, and you should contact your doctor for specific medical advice matching your individual needs.**
A snapshot from a post-class track workout, Spring of 2018
March 2022
Spring is on the horizon. The weather is warming up and trees are blossoming. Historically, spring has always been associated with outdoor track season and the chance to step into the 400m. Oval Office to throw down. Since 2020 however, spring has been marked with the absence of outdoor track racing, both due to the COVID-19 pandemic and due to my chronic injury. Day in and day out, I attend to my rehabilitation, making adjustments based on new information and perspectives that shed light on my condition.
One of my colleagues, who is also a residency trained physical therapist, was kind enough to perform an evaluation on me and begin a plan of care independent of the one I had ongoing with the PT at the previously mentioned clinic. My rehabilitation program has been modified to better fit my condition, and at the time of this writing includes only a fraction of the exercises provided by my first PT. Quantity does not always equal quality, as the positive benefits from my new PT program have started to produce small but tangible improvements to my condition that outweigh the program from my first PT (If you are interested in the program that I have currently, you can scroll to the bottom of the page where there is an addendum).
The biggest changes occurring are the improvements in strength of my extensor hallucis longus muscle (which receives nerve contribution from the L4, L5 and S1 nerve roots)1, and that my symptoms are starting to centralize. I’ll break down briefly why each of these pieces is important.
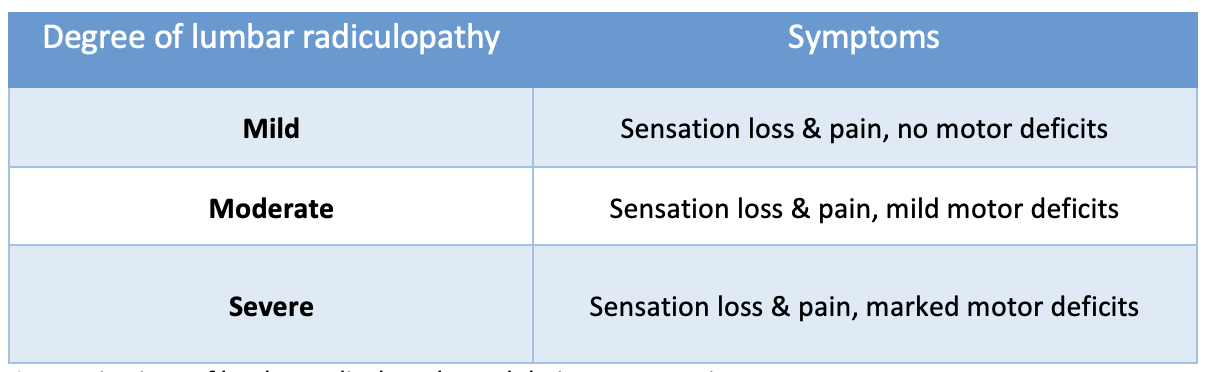
Lumbar radiculopathy can be categorized into 3 broad categories: mild, moderate and severe, each with defining features: (2)
Categorizations of lumbar radiculopathy and their accompanying symptoms
A key note from the table: more muscle strength loss means that the lumbar radiculopathy is worse, and improving muscle strength indicates that the lumbar radiculopathy is getting better.
My case of back pain with concurrent leg symptoms is one example of how pain starting in the low back can create symptoms in other places away from the center of the body. Centralization refers to a phenomenon where the pain starts to move back towards the midline of the spine in response to repeated movements or guided positioning.(3) Centralization is a positive response to treatment, as pain can be diminished or eliminated entirely. (3)
Although I was able to manage my pain a little bit better when I go about my daily routine, it was still very difficult to walk outside my house for anything longer than a quarter mile nonstop, and trips lasting longer than 2 hours outside of the house were still daunting. Such is the nature of rehabilitation for chronic injuries: one cannot rush the process. Just like with building competition fitness, the process must be completed one step at a time, with patience and with gratitude.
In late March, I went in to receive my epidural steroid injection. My mother was kind enough to drive me to the surgery center and back. Preoperative procedures included paperwork and health screenings. As I sat waiting, I thought about how long my overall journey has been thus far, and wondered about how I would feel after the injection medication had settled in.
The operation itself took about 15 minutes. I had a choice between only doing the local anesthetic or getting an IV with medications for anesthesia and anxiety reduction. I chose to just do the local anesthetic and remained conscious for the whole procedure. The most uncomfortable portion of the procedure was the end when the medication was being injected. Even with the local anesthetic, I still had a series of stabbing pains in my right low back and SI joint area. Those stabbing pains were accompanied by surges of pain down the back of my thigh and calf, and then it was done.
Waiting in the pre-operative room.
I returned to the pre-operative room to have my blood pressure taken again and to wait the designated recovery time before going home. As a nurse took my blood pressure, she asked me what sport I did. We talked about running, and she shared her history of running half marathons and a couple marathons, and how she loved running but had to cut back due to her hip. One of my favorite things about the sport of running is that no matter what level one is at, everyone shares a similar love and appreciate the profound impact it can have on their daily life. It was nice to have that brief connection again.
Once recovered enough, I returned home and proceeded to relax for the next couple days, taking my time with my rehab exercises and daily tasks as able. I was very sore the day of, and with each passing day, the soreness gradually improved.
----------------------------------------------------------------------------------------------------------------------------------------------------------------
April 2022
I have started to notice the effects of the combination of the epidural steroid injection and PT in subtle yet tangible ways. At the beginning of the month, I went out to the Stanford Invitational to meet with my college coach as well as to watch a small contingent of UCCS athletes make attempts on school records (click here to read the full meet recap). I was out of my house for a cumulative 8 hours, from mid-afternoon until midnight. In this past winter, attempting something like this would have not only been extremely painful, but also would have required multiple days at home to recover. I was impressed to wake up the day after the meet and to not be nearly as sore as I thought I would be.
With each week that passes, I continue to attend to my PT daily. I have started to note that my capacity to leave the house for certain errands and tasks has improved a little bit, but my body is still nowhere near being ready to run, which I am okay with. Rehabilitation is all about making overall steady progress, and with consideration to the length of time that I’ve been injured, any progress is good progress.
My biggest test of overall function begins this month as I return to work as a physical therapist. I will need to be able to function enough to walk around, lift objects, and treat patients for 40-hour work weeks. Commute time will put my time out of the house closer to around 50 hours or so per week. This is going to be a significant change from my current daily schedule, but if my body can continue to progress despite working full time, this will be a big win for me. One day at a time.
Thanks for following along so far, stay tuned for the next installment of the series!
References
1. Lezak B, Summers S. Anatomy, Bony Pelvis and Lower Limb, Extensor Hallucis Longus Muscle. [Updated 2021 Oct 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539875/
2. Dydyk AM, Khan MZ, Singh P. Radicular Back Pain. [Updated 2021 Nov 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546593/
3. Albert HB, Hauge E, Manniche C. Centralization in patients with sciatica: are pain responses to repeated movement and positioning associated with outcome or types of disc lesions?. Eur Spine J. 2012;21(4):630-636. doi:10.1007/s00586-011-2018-9
----------------------------------------------------------------------------------------------------------------------------------------------------------------
Addendum
This section is just to explore a little more of my rehabilitation process. If I were to make a list of primary impairments that needed to be addressed, it would include a left lateral shift, decreased lumbar extension range of motion, and increased neural sensitivity of the sciatic nerve. The exercises that I used at the start of my rehab include:
- R. sciatic nerve glide w/ my body positioned in a lumbar rotated position, R. side up
- Side left pelvic glides in a left side-leaning position
- Romanian Deadlift with a light weight (to serve as a loaded sciatic nerve glide)
By the end of April, the left lateral shift has mostly improved, but would still return at the end of a work day. I am also still having difficulties with full lumbar extension and neural sensitivity. The program has now progressed to:
- R. sciatic nerve glide w/ my body positioned in a lumbar rotated position, R. side up
- Sciatic nerve glide in supine, using ankle motion to stress the sciatic nerve
- Side plank dips (serving as a side glide progression), performed on both sides
- Side glides using an elbow to stabilize the thoracic spine (to put more emphasis on the lumbar spine during shift corrections)
- Traditional Deadlift with 45 lb. weight
- Prone press-ups and bridges to move into lumbar extension
I haven’t included any specifics in sets or reps, as those can vary from day to day depending on how my nervous system is feeling. On better days, I’ll do more as my body is able to manage, and then make adjustments to the cumulative load on the days where my body is not quite feeling it. Similar to training competitively for running, just not nearly as exciting :P
My plan for return to work also includes a graded exposure program where I track my cumulative time in sitting or semi-upright position (my clinic has adjustable standing desks that I can hunch over). Time will tell as to how my body responds to this, but based on clinical experience, I think it should work.